10 Quirks That Might be Autism: Rating Pain
Part 5: In these 10 quirks about me, you’ll see many shades of autism.
This post is part of the series 10 Quirks About Me.
Rating pain on a scale is an agonizing task, and it’s one that I’ve had to repeat frequently. You might be wondering how this is one of the 10 quirks about me that might be related to my autism. But not being able to communicate the amount of pain effectively is an issue that is part of autism’s core. To compound that issue, people with autism have a different response to pain than neurotypical people. And you’re about to find out just how much trouble those problems have caused me.
I am sharing these stories in the series 10 Quirks About Me to help people understand autism spectrum disorder and its effects. But these traits do not make you autistic. If you believe that you would benefit from an autism diagnosis, please seek one from a qualified professional. You can get more information about autism spectrum disorder from the National Institute of Health (NIH), the Center for Disease Control (CDC), and advocacy groups such as Autism Speaks.
Now, I’ll try to make the discussion on rating pain as painless as possible.
Everybody Hurts, Sometimes
In 2003, I was in a car crash that has led to seven surgeries on my spine. So, I visit a pain specialist every month because I am a chronic pain patient. That means that I regularly have to rate my pain using a scale that measures it from 0 (none) to 10 (worst possible). I’m able to use the scale effectively now. But that has not always been the case.
You’ve probably has heard of the pain scale or seen it at least once in your life. But if not, you can read more about it here. Even if you are one of the neurotypical people who has problems choosing from the 11 different numbers on the scale, you probably can do it accurately if you’re being honest. And once the conversation about the pain scale is over, you probably never give it a second thought.
Then, there is me. That pain scale is torturous, and I can’t let it go. I’ll worry about the answer that I gave throughout the rest of the appointment. Then, I’ll think about it more on my way home. Sometimes, I’m still wondering if I chose the right number on that pain scale many weeks after I chose it. At least, that’s the way it used to be.
What Hurts the Most
I’ll try to explain how this is a problem. Suppose for a minute that I’m visiting the doctor, and I have pain. The nurse has taken vitals. Now, he wants me to tell him how much pain I’m feeling.
He asks, “On a scale from 0 to 10, how would you rate your pain?”
There’s a chart hanging on the wall, and it looks like this:
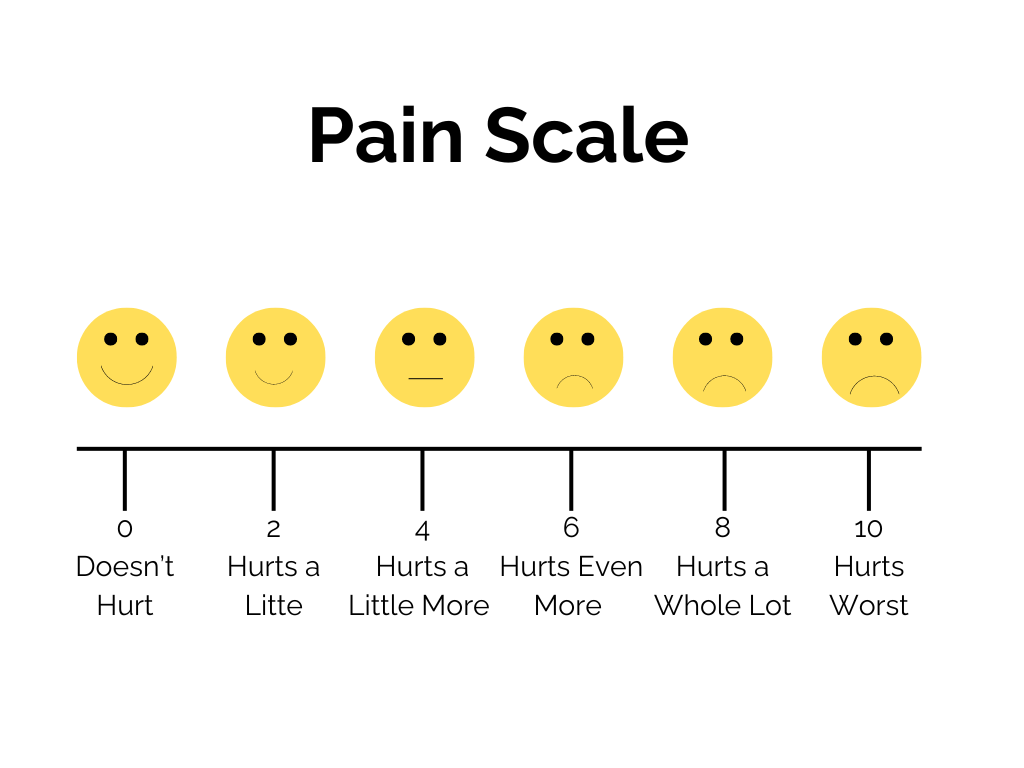
The first thing that I see are the faces. The words and numbers below them haven’t even entered my mind before I’m already feeling stress. The smiles and frowns on those faces are not much different. I’ll begin to wonder, is my frown that big? I can’t read the expressions.
Before I can answer that question, I see the words. In my world, ambiguity cannot exist, and words such as “a lot” and “even more” are vague. Then, I wonder how much “a little pain” is relative to. But the only help I get are the other words on the chart. Those present the same problem. Finally, I’m at the numbers. Numbers are OK with me, but not when you put the facial expressions and words with them. And what about the numbers that are missing? That’s when I start to panic.
You Don’t Know How It Feels
The thought process that I’ve just described occurs during a period of a few seconds. Now, here’s the tricky part: I could compensate for all of it most of my life. Because I also have exceptional and very fast reasoning and language skills, I could give an answer quickly. That’s less common in autism and more likely related to my complete diagnosis, which you can read about in my first post about autism.
Besides, being able to give an answer quickly didn’t make it right. I would spew a long-winded answer that could be confusing or nonsensical. It also didn’t answer the question. Most medical professionals want a number, so I learned to say “11.” Some nurses would laugh, and others would groan. In fact, I did this from the time I was first asked to rate my pain at the age of 13 until I was 37.
Then, in June 2014, I was in a pain doctor’s office in Quincy, Illinois. They had a more detailed pain scale. It was exactly what I needed to be able to relate to the pain. Instead of telling me that I needed to correspond the number to an emotion, this chart showed how the numbers corresponded to real-life injuries. For example, a 10 was the loss of a limb and a 2 was a pinch.
Comfortably Numb
More than anything, it’s a relief. I don’t have as much anxiety about rating my pain anymore. It might not seem like a big deal to be unable to report pain effectively, but it can be a matter of life or death.
I was out of touch with my pain for many years. Sometimes I wasn’t reporting the pain, so the doctors didn’t know how to treat me. Others, I was overstating how much pain I was in. In those situations, doctors frequently prescribed more pain medication than I needed. Some of that medicine is dangerous when taken in large quantities, and I probably was in the danger zone more than once. Besides, no one should take pills that they don’t need.
That doesn’t happen now. I’m able to correctly articulate my pain most of the time because I know what the numbers really mean. My range is about 2-7, with 2 being about my normal and 7 being about as bad as it gets for me, briefly, after surgery. I don’t think that’s so bad. It’s also logical, and it’s something my doctors can work with.
Catch the rest of the series: 10 Quirks About Me